April 2025 | Michael Fechter
Growing up in Quincy, a small town about 25 miles west of Tallahassee during the 1960s and ’70s, Alma Littles “witnessed a lot of illness and death.”
When she was 14, her father complained he was having trouble breathing. “By the time ambulance arrived, it was too late.” An older sister gave birth to twins at home — one died nine days later, and her sister died about two months after that from a pulmonary embolism, likely related to the childbirth. Another sister lost a baby boy at 2 weeks old due to jaundice and dehydration.
Routine preventative care, the kind most people enjoy, could have helped save those lives, she says. But Littles doesn’t remember seeing a family doctor. The school nurse took care of her, including providing her childhood vaccinations.
Those experiences set her on a path to becoming a doctor, helping to care for those underserved communities, including her hometown. When Florida State University came calling to help staff its new medical school in 2000, Littles initially hesitated because she liked what she was doing.
But FSU’s mission statement, imposed by the Florida Legislature, specifically mandates teaching students to “practice patientcentered health care … especially through service to elder, rural, minority and underserved populations.”
“That is my personal, professional mission statement,” Littles says. She joined FSU’s faculty, creating and running a department of family and rural health until last summer, when she became dean of the College of Medicine. FSU students train in poor, underserved communities such as Marianna and Immokalee. Littles recruits people from rural communities to become doctors and then return home to practice.
That’s what Laura Davis did.
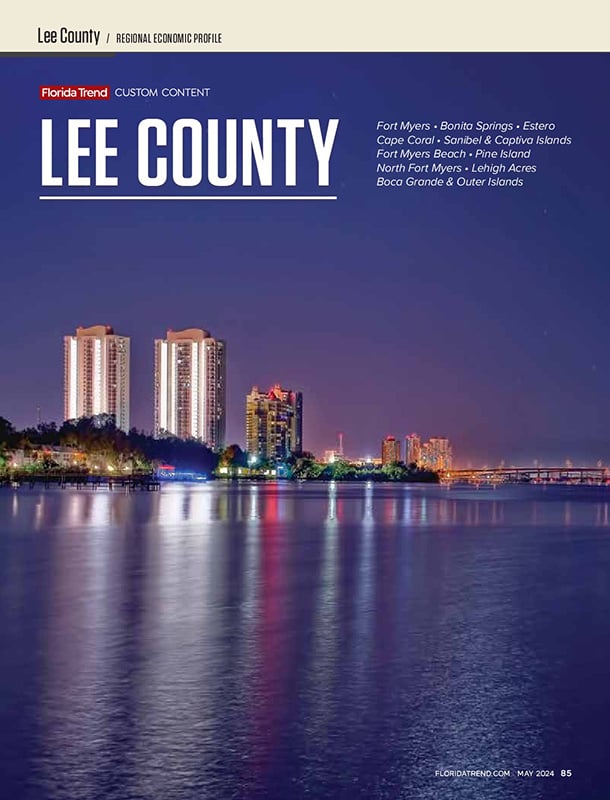
Davis, 41, grew up in Blountstown, Calhoun County’s county seat, about 48 miles west of Tallahassee just west of the Apalachicola River. “Most of the time when I grew up, we just had two traffic lights,” she says. “We have several more now.”
It’s a close-knit community where “people have known each other’s families for generations. Lots of times we joke, you may not know people’s names, but you know where their mama’s house was.”
Calhoun County has about 13,800 people and 11 total physicians. There are no pediatricians, no OB/GYNs. Davis is one of four practicing family medicine, working for TMH Physician Partners. The practice and nearby Calhoun Liberty Hospital are Tallahassee Memorial Healthcare affiliates.
“Our practice here is literally cradle to the grave,” she says. “I saw a 3-day-old today and will go to the nursing home to see a 99-year-old before the week’s over with. So it’s just that whole literal span of a lifetime, which is really interesting and really fun.”
Calhoun Liberty provides lab work and imaging, but patients needing specialists may wait weeks and drive 30 minutes to an hour to be seen. “It’s just the nature of being in a rural community,” Davis says.
Long Waits Everywhere
As Florida’s doctor shortage worsens, however, those waits affect population centers, too, says Florida Hospital Association President Mary Mayhew. “There are areas of the state where you have great insurance coverage, you’re new to the area and you could wait six months or more to get a primary care appointment.” This can force some patients into emergency room visits, which can drive up costs.
Primary care physicians represent more than a third of the 18,000 doctors Florida may need in the next decade. But “we’ve reached a point in this country and in this state where we need more of almost everything, almost every specialty,” Littles says.
That’s where graduate medical education and residency slots become vital to “grow” the next generation of doctors. But federal funding from Medicare was set in 1996 and, because it has not been adjusted substantially since, ignores population shifts. So growth states like Florida have fewer doctors-in-training per capita than they did nearly 30 years ago, while states losing population have disproportionately more resident doctors.
At the time, there was “concern that there was an oversupply of physicians,” a U.S. Senate Bipartisan Medicare GME Working Group statement said last year. The group is pushing legislation to add 14,000 new Medicare-funded residencies at 2,000 per year for seven years, but it hasn’t made it out of the finance committee.
As a result, Florida graduates more young doctors than it has residencies, forcing many to leave the state for training. Most don’t come back.
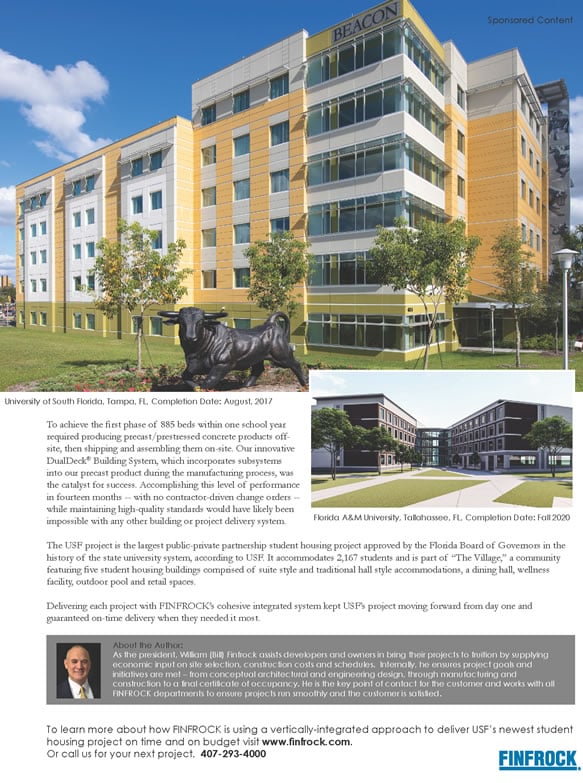
Calhoun County, a rural county in the northern Panhandle, has about 13,800 people and 11 physicians. There are no pediatricians and no OB-GYNs.
Making Headway
Florida lawmakers last year tried to step into the void, passing a package of bills dubbed “Live Healthy.” It includes loan forgiveness for doctors who treat underinsured, underserved communities. But the biggest investment added $62 million to “Slots for Doctors,” which provides $100,000 for new residency slots in the state. It builds on the program established in 2023 and could add 880 new trainees.
Advocates say most medical residents stay in the communities where they train, often within the same hospital that brought them in.
BayCare, a health network covering Hillsborough, Pinellas, Polk and Pasco counties, is banking on that track record to ensure its future staffing needs, says Chief Physician Executive Sowmya Viswanathan.
BayCare decided to pursue more residency positions aggressively before Slots for Doctors was passed, and already has grown from 30 residents to 200, with ambitions of reaching 650 by 2029. If two-thirds of those residents stay in the system after completing their training, “I’m golden,” Viswanathan says.
In the Panhandle, Tallahassee Memorial Healthcare is working with FSU Health to expand training programs and bring care closer to the region’s small towns, says President Mark O’Bryant. That includes working with the St. Joe Co. To build a new hospital in Panama City Beach that should be eligible for additional residency slots.
The state-funded residencies are a step in the right direction, FSU’s Littles says, and it’s encouraging that lawmakers are aware of the burgeoning physician shortage.
“I am optimistic that we’ll continue to make some headway,” she says. “It’s certainly not happening as fast as I’d like to see it.”